New PV Loop Guidelines: Setting the Standard for Rodent Cardiac Research
New PV Loop Guidelines: Setting the Standard for Rodent Cardiac Research
A new consensus guidelines paper in the American Journal of Physiology – Heart and Circulatory Physiology marks a major step forward in standardizing best practices for researchers using pressure-volume (PV) loops to assess cardiac function in rodents.
The paper, “Guidelines for Assessing Ventricular Pressure-Volume Relationships in Rodents“ provides a comprehensive framework for best practices in surgical techniques, data collection, analysis, and interpretation—aimed at improving rigor, reproducibility, and cross-study comparability in cardiovascular research.
The guidelines were co-authored by a team of leading cardiovascular researchers, including two members of the Endpoint Preclinical Expert Network, Dr. Oliver Wearing and Dr. Tim Hacker, along with Dr. Chris West, who serves as the host and head instructor of our Rodent PV Loop Masterclass.
- Dr. Oliver Wearing – Lead Surgical Instructor for the Rodent PV Loop Masterclass and a consultant in PV loop methodologies, specializing in microsurgical techniques for various cardiovascular models.
- Dr. Tim Hacker – Expert in cardiovascular research and hemodynamics, with a focus on LV and RV PV Loop applications, disease models, and complementary imaging technologies.
- Dr. Chris West – A leading researcher in pressure-volume loops and integrative physiology; host and head instructor of Endpoint Preclinical’s Rodent PV Loop Masterclass.
Congratulations to the entire group that contributed to this essential resource. You can learn more about the authors and their research via the links below.
- Naomi C. Chesler – Department of Biomedical Engineering, University of California, Irvine
- Mitchel J. Colebank – Department of Mathematics, University of South Carolina
- John N. Lorenz – Department of Pharmacology, Physiology, and Neurobiology, University of Cincinnati
- Jeremy A. Simpson – Human Health & Nutritional Sciences, University of Guelph
- Christopher R. West – Centre for Chronic Disease Prevention and Management, UBC Okanagan
What the Guidelines Cover: Addressing Variability and Improving Standards
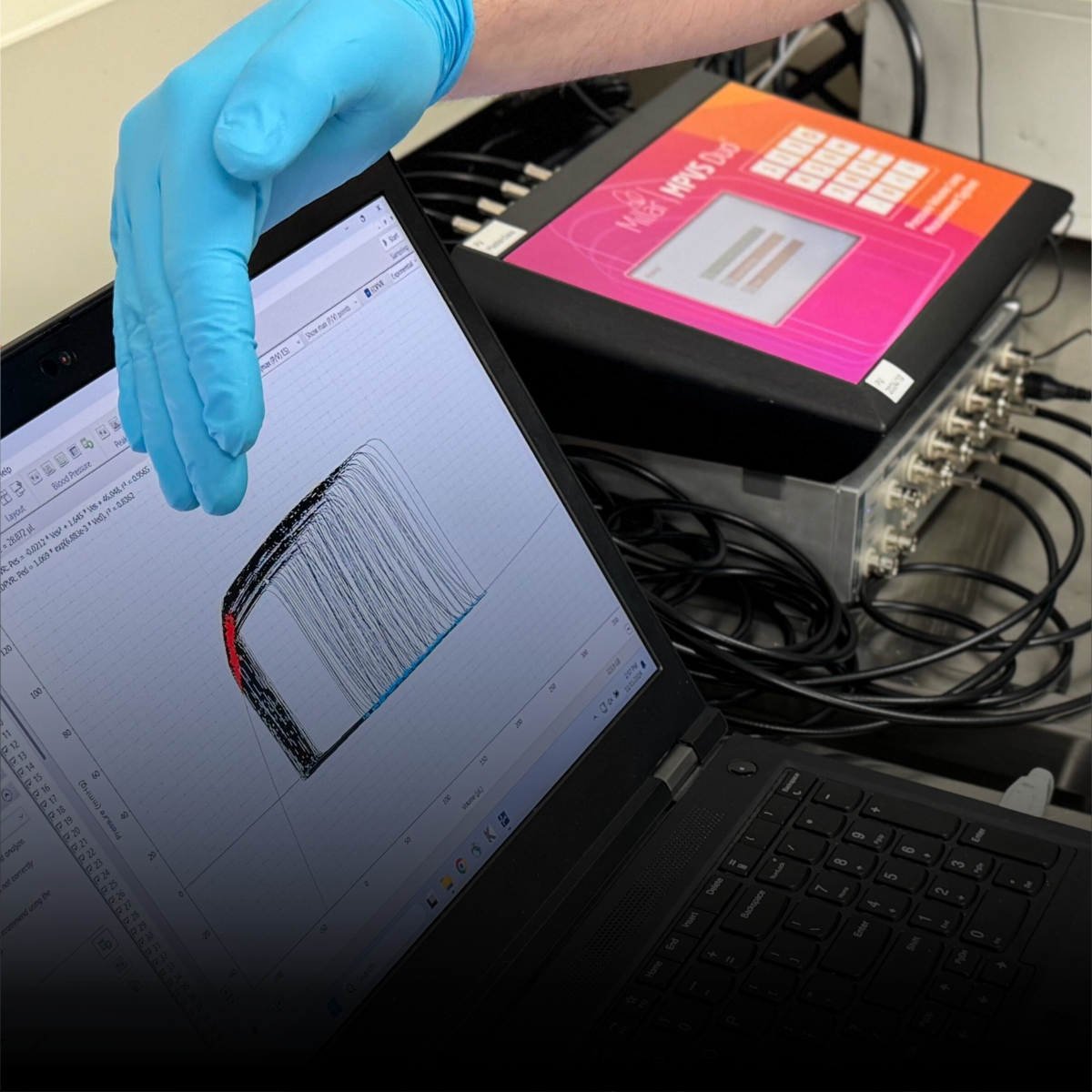
The PV loop method is a gold-standard technique for assessing in vivo cardiac function, allowing researchers to obtain load-independent indices of systolic and diastolic performance. However, inconsistencies in study design, execution, technologies and reporting have historically undermined reproducibility in the field.
This guidelines paper seeks to resolve these challenges by covering:
- A comprehensive survey of recent rodent PV studies, highlighting inconsistencies in data reporting
- The impact of anesthesia choices on cardiovascular function and PV loop data quality
- Best practices for volume calibration, including conductance and admittance methodologies
- Guidelines for steady-state data collection, ensuring high-quality baseline PV recordings
- A standardized approach to measuring load-independent indices of systolic and diastolic function
Survey of Recent Rodent PV Studies: A Call for Standardization
One of the most revealing aspects of this paper is a survey of 56 rodent PV studies published in AJP – Heart and Circulatory Physiology over the past decade. The survey evaluated how consistently key methodological details were reported, including:
- Anesthesia protocols
- Temperature control measures
- Use of mechanical ventilation
- Calibration techniques for volume measurements
- Data reporting standards
Less than half of the studies provided complete methodological details, despite their significant impact on data reliability. For example, only 64 percent of studies confirmed performing appropriate volume calibration, a fundamental step in ensuring PV data validity. The survey underscores why established guidelines are so critical—by setting a clear standard, the authors aim to eliminate methodological inconsistencies and elevate the reliability of PV loop data across research labs worldwide.
Volume Calibration: Conductance vs. Admittance Approaches
Accurate volume calibration is essential to ensure PV loop data reflects true cardiac volumes. The guidelines compare and contrast the two methods:
Conductance Volume Calibration:
- Uses hypertonic saline or dual-frequency techniques to account for parallel conductance.
- Requires external validation (e.g., echocardiography, flow probes) to establish stroke volume.
- Assumes a constant parallel conductance value
Admittance Volume Calibration:
- Separates blood conductance from myocardial tissue contribution in real time.
- Reduces the need for post-hoc volume correction.
- Still requires independent stroke volume validation (e.g., echocardiography, flow probes).
The paper emphasizes the importance of precise volume calibration, highlighting that failure to calibrate properly leads to significant measurement errors in ventricular function assessment.
Best Practices for Steady-State PV Data Collection
Before assessing load-independent function, PV loops must be recorded under baseline, steady-state conditions. The guidelines recommend:
- Sampling at a minimum of 2 kHz to ensure accurate waveform resolution
- Recording multiple cardiac cycles to account for beat-to-beat variability
- Avoiding drift in catheter placement to prevent artifacts in volume measurements
- Reporting full data distributions, rather than just mean values, to capture physiological variability
Load-Independent Indices of Systolic and Diastolic Function
A major strength of PV loop studies is the ability to assess cardiac function independent of loading conditions. However, achieving truly load-independent indices requires careful manipulation of preload and afterload, precise data collection, and proper analytical techniques. The guidelines establish best practices for deriving load-independent indices, including:
- End-Systolic Elastance (Ees) – The gold-standard index of contractility, but requires careful modeling to avoid misleading conclusions.
- Preload-Recruitable Stroke Work (PRSW) – A highly sensitive marker of systolic performance that accounts for variations in ventricular filling.
- End-Diastolic Pressure-Volume Relationship (EDPVR) – A key indicator of ventricular compliance and diastolic function, requiring careful afterload manipulations.
The guidelines address four critical questions researchers must consider when performing pressure-volume loop manipulations:
- For how long should I occlude the inferior vena cava (IVC), and how many times should I repeat these occlusions?
- How do I know when I have a good family of PV loops?
- Should I also perform abdominal aortic occlusion (AAO) in addition to IVC occlusion?
- What measures can I derive from IVC/AA occlusions to assess systolic and diastolic function?
By following the best-practices described in the guidelines, researchers can ensure their load-independent PV loop data is robust, accurate, and reproducible, ultimately improving the translational impact of rodent cardiac research.
Anesthesia Choices: A Critical Influence on PV Loop Data
Anesthesia plays a major role in cardiovascular function, yet its impact on PV loop measurements is often underestimated. The guidelines paper provides an in-depth review of the effects of different anesthetics, including:
- Isoflurane – Most commonly used, provides stable anesthesia but acts as a vasodilator, which can impact ventricular loading conditions, particularly in right ventricular studies.
- Barbiturates (e.g., pentobarbital) – Depresses sympathetic tone and myocardial function, which can reduce contractility and alter hemodynamic parameters.
- Urethane – Long-acting anesthesia that preserves autonomic reflexes, making it more suitable for studies requiring stable baseline cardiovascular function but has limitations due to toxicity concerns.
Careful selection of anesthetic type, dose, and delivery method minimizes confounding variables, ensuring accurate and reproducible PV loop measurements.
These new guidelines represent a major step forward for rigor and reproducibility in PV loop studies. By integrating these best practices, researchers can elevate the quality of their data and drive impactful discoveries in cardiovascular physiology. Congratulations and thank you to the authors and all that contributed to creating this essential resource. Access the full paper here.
Expert Consulting for PV Loop Studies
In addition to our Masterclass, Endpoint Preclinical offers expert consulting services and technology access to support researchers at every stage of their PV loop studies. Our team provides specialized guidance in:
- Surgical services – Expert catheter placement for high-fidelity PV loop data acquisition
- Data acquisition and analysis – Ensuring reproducible, high-quality pressure-volume measurements
- Disease model creation – Custom experimental designs for cardiovascular research
- Complementary techniques – Integrating echocardiography and other imaging modalities to enhance study outcomes
Whether you need hands-on support for surgical procedures, help with study design and data interpretation, or guidance on integrating PV loops into your preclinical research workflow, we are here to help. Contact us today to learn how we can support your study objectives.